60 YEARS OLD FEMALE WITH SOB
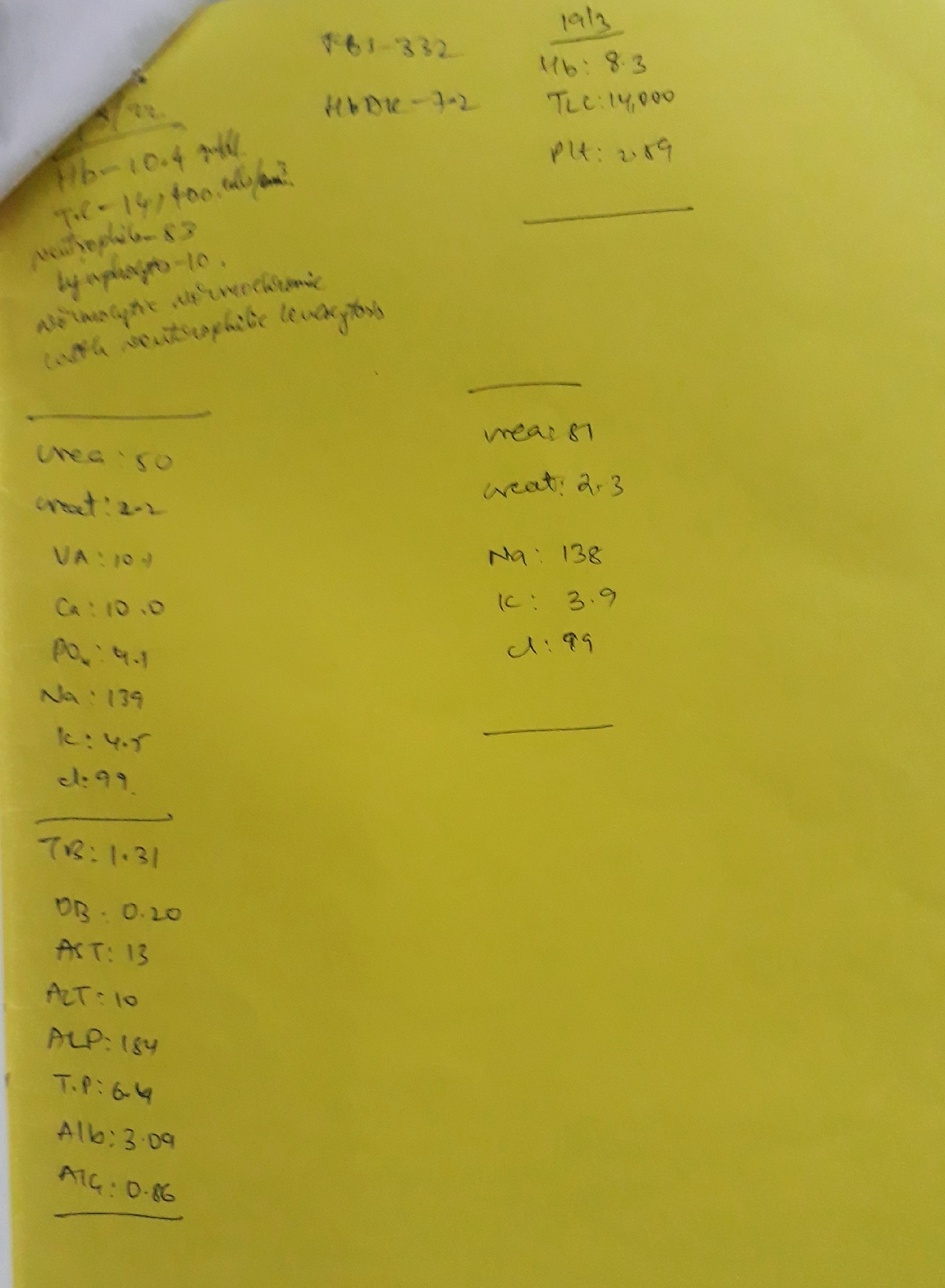
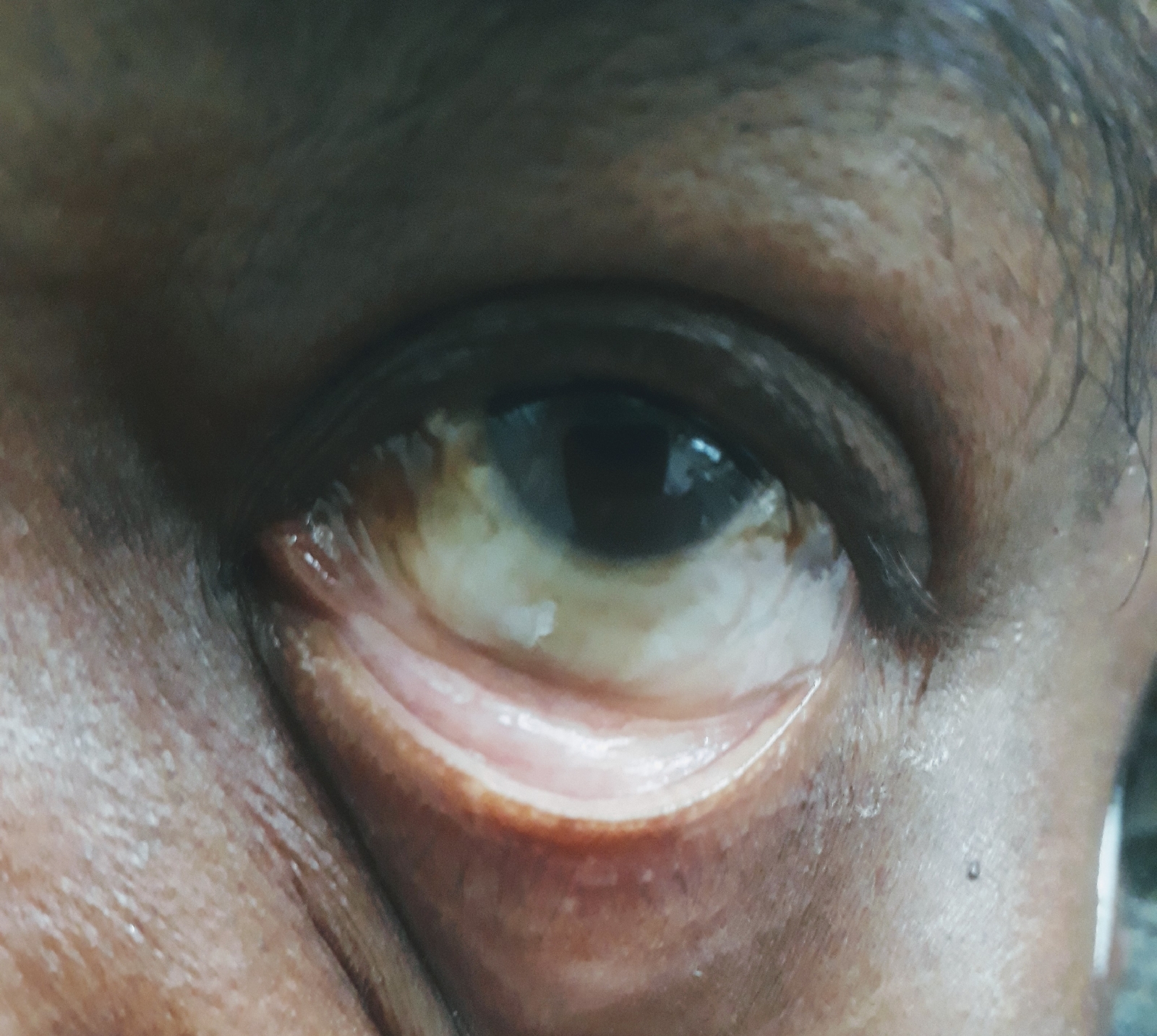
60 YEARS OLD FEMALE WITH SOB CASE DETAILS 60 year old female patient came with c/o SOB since 3 days SOB ( grade III progressed to grade IV ) over 3 days Aggravated while lying down (orthopnea ) HISTORY OF PRESENT ILLNESS Pt. was apparently asymptomatic 3 days back then developed SOB ( grade III progressed to grade IV ) over 3 days Aggravated while lying down (orthopnea ) No c/o cough, fever, vomiting, loose stools No c/o pedal edema PAST HISTORY K/c/o HTN SINCE 10 YEARS and on medication ( metoprolol & Amlodipine tab. ) DM since 5 years and on medication ( metformin & glimiperide tab.) Not k/c/o CAD, TB, EPILEPSY PERSONAL HISTORY DIET - MIXED APPETITE - NORMAL SLEEP - INADEQUATE BOWEL & BLADDER - REGULAR NO ADDICTIONS GENERAL EXAMINATION VITALS Pt. Is c/ c/ c Temp - Afebrile B.P. - 160/ 80 mm Hg P.R - 102 bpm R.R - 15 cpm GRBS - 340 mg /dl Spo2 - 95 % @ 5 lt o2 PHYSICAL EXAMINATION PALLOR...